Coronary Artery Disease
Coronary artery disease limits blood flow in your coronary arteries (arteries), which carry blood to your heart muscle. Cholesterol and some other substances form plaques that narrow your coronary arteries and begin to cause symptoms as they grow into the vessel. Chest pain is the most common symptom of coronary artery disease. If left untreated, it can lead to heart attack, heart rhythm disturbances or heart failure. However, it should not be forgotten that there are many treatment options available for this disease today.
What is Coronary artery disease or Coronary artery disease?
Coronary artery disease is the narrowing or blockage of your coronary arteries, which supply oxygen and nutrient-rich blood to your heart. This is because plaque (including cholesterol) builds up in these arteries over time. As a result, it causes the required amount of nutritious, oxygen-laden blood not to reach your heart muscle.
We can compare the stenosis in the coronary arteries to a road that merges due to repairs and reduces to a single lane. Traffic continues to flow, but it is slower and not enough vehicles can get to their destinations on time. However, in some cases with coronary artery disease, you may not notice anything until the plaque triggers a blood clot and momentarily creates a complete blockage. A blood clot is like a concrete barrier in the middle of the road, causing traffic to come to a complete halt. Similarly, blood cannot reach your heart, resulting in the death of heart cells that cannot be fed at all, causing a heart attack.
You may have coronary artery disease for many years and have no symptoms until you have a heart attack. That’s why coronary artery disease is also called a “Silent Killer”.
Other names used for coronary artery disease include “Coronary Heart Disease”, “Cardiovascular Disease” and “Ischemic Heart Disease”. Additionally, when most people use the general term “Heart Disease”, what they mean is “Coronary Artery Disease”, the most common heart disease.
Types of Coronary Artery Disease
There are two main forms of coronary artery disease:
1)Stable Ischemic Heart Disease: This is the chronic form. Your coronary arteries gradually narrow over the years. Over time, your heart receives less blood containing oxygen and nutrients. You may feel some symptoms, but most of the time this does not prevent you from living your daily life.
2)Acute Coronary Syndrome: This is the sudden form (also called Heart Attack, Myocardial Infarction), which is a medical emergency. The plaque in your coronary artery suddenly ruptures on its own, and a blood clot forms inside your artery, completely or almost completely blocking blood flow to your heart. This sudden blockage causes a heart attack, which progresses to life-threatening situations if the heart’s blood flow is not restored by intervening and opening the vessel as soon as possible.
How common is coronary artery disease?
Coronary artery disease is a very common disease. It is thought that approximately 350 million people worldwide have coronary artery disease. And its incidence is increasing with the aging world population. It continues to be the most common cause of death all over the world.
What are the basic symptoms?
Even if you have coronary artery disease for a long time, you may not have symptoms. It can take years, even decades, for plaque to accumulate and grow in the vessel wall. However, you may notice mild symptoms as your arteries narrow. These symptoms mean that your heart is not adequately delivering oxygen and nutrient-rich blood to its own tissue and to your body, or sometimes it is having to work harder to deliver it.
Chronic coronary artery disease symptoms mainly include:
1-Stable angina (Chest pain): This is the most common symptom. Stable angina is temporary chest pain or discomfort that comes and goes in a predictable pattern. You usually notice it during physical activity or emotional stress. Its severity decreases or disappears completely when you rest or take a medication such as nitroglycerin (a very short-acting vasodilator that relieves angina).
2-Shortness of breath (dyspnea): Some people feel short of breath during light physical activity. This is considered a sign of coronary artery disease, even if it is not accompanied by pain.
In addition to these basic symptoms, fatigue, dizziness, pain in the jaw, neck or arms or even the back during exertion, a feeling of fullness, a feeling of pressure may also be symptoms of coronary artery disease.
However, it should not be forgotten that sometimes the first symptom of coronary artery disease may be a “Heart Attack (Myocardial Infarction”).
What is the cause of coronary artery disease?
Atherosclerosis, that is, arteriosclerosis, is the direct cause of coronary artery disease. Atherosclerosis is the gradual build-up of plaque in the arteries (arteries) in your body. When plaque affects blood flow in your coronary arteries, you have coronary artery disease.
Records; It consists of cholesterol, waste products, calcium, and fibrin (a substance that helps your blood clot). As plaque accumulates along your artery walls, your arteries become narrower and harder (hence also described as atherosclerosis). Plaques can damage your arteries by blocking them, which limits or stops blood flow to a particular part of your body. When plaque builds up in your coronary arteries, your heart muscle can’t get enough blood. Thus, your heart cannot receive the oxygen and nutrients it needs to function properly (myocardial ischemia). This causes chest discomfort (angina) and puts you at risk of heart attack. People who have plaque buildup in their coronary arteries often have plaque buildup elsewhere in their bodies. This can lead to conditions such as “Carotid Artery Disease (carotid artery disease)”, “Renal Artery Disease (kidney vascular disease)” and “Peripheral Artery Disease (disease of the vessels leading to the arms, legs and other organs)”.
Is coronary artery disease genetic?
Partially yes. Family history increases your risk of coronary artery disease. But many other risk factors have nothing to do with your genetics. The choices you make every day (such as smoking, poor diet, sedentary lifestyle) have a greater impact on your risk of coronary artery disease.
What are the risk factors for coronary artery disease?
There are many risk factors for coronary artery disease. You can’t change all of these. But you can manage some by making lifestyle changes or taking medication. The most important point is to determine with your doctor what you can do about these risk factors.
Let’s take a detailed look at the risk factors:
- Being over 45 for men and 55 for women.
- Having a biological first-degree family member with heart disease. Especially a father or brother diagnosed before age 55, or a mother or sister diagnosed before age 65.
- Consuming too much saturated fat or refined (processed) carbohydrates.
- Not getting enough exercise (at least 150 minutes a week for women and at least 300 minutes for men).
- Not getting enough sleep (at least 7 hours for adults).
- Using cigarettes, electronic cigarettes or other tobacco products.
- Presence of atherosclerosis (hardening of the arteries) in non-cardiac vessels.
- Having high blood pressure.
- Having high levels of LDL (“bad”) cholesterol.
- Having low HDL (“good”) cholesterol levels.
- Having high triglyceride levels (hypertriglyceridemia).
- Presence of anemia.
- Almost all rheumatic diseases, including Lupus and Rheumatoid Arthritis.
- Chronic kidney disease (failure)
- Diabetes
- HIV/AIDS.
- Metabolic syndrome. Especially a body mass index (BMI) higher than 25.
- Sleep disorders such as sleep apnea.
- Migraine
- Early menopause (before age 40).
- Endometriosis and Polycystic Ovary Syndrome.
- History of gestational diabetes, Eclampsia or Preeclampsia.
- Hormonal birth control use.
What are the complications (greater harm it may cause) of coronary artery disease?
The main complication of coronary artery disease is a heart attack. This is a medical emergency that can be fatal. In this suddenly developing condition, cells begin to die with each passing second because your heart muscle cannot receive enough blood. You need emergency surgery to open your vein to restore blood flow to your heart and save your life. Even if it doesn’t develop suddenly, over the years, disease in your coronary arteries can weaken your heart and lead to life-threatening complications, including:
- Arrhythmias (atrial fibrillation and other dangerous heart rhythm disorders)
- cardiac arrest
- cardiogenic shock
- Heart failure
How is coronary artery disease diagnosed?
Essentially, physicians diagnose coronary artery disease through physical examination and tests. During your physical examination, your physician: Measures your blood pressure. He listens to your heart with a stethoscope. It asks what symptoms you are experiencing and for how long. Asks for your medical history. It asks about your lifestyle. It asks about your family history. He or she will want to know if there was heart disease between your biological parents and siblings. All this information will help your doctor determine your risk of heart disease. Ultimately, he will decide which tests to do.
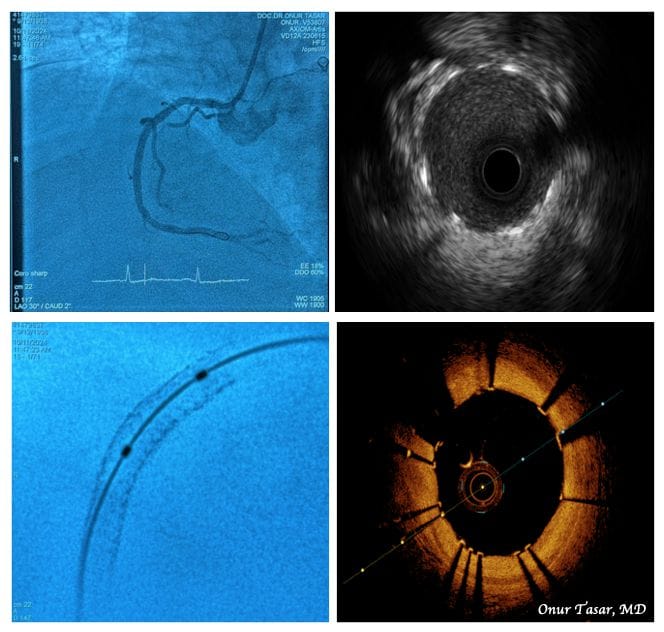
Which tests are used in the diagnosis of coronary artery disease?
Your doctor may also recommend one or more tests to evaluate your heart function and diagnose coronary artery disease. These:
- blood tests
- Electrocardiography (EKG)
- Echocardiography (ECO, i.e. Heart Ultrasound)
- Myocardial Perfusion Scintigraphy
- Heart MRI (EMAR, Magnetic Resonance Imaging)
- Virtual Angiography with Computed Tomography (CT)
- Invasive Coronary Angiography (Classical Heart Angiography)
- Coronary Calcium Screening
- Exercise Stress Test (Exertion Test)
How is coronary artery disease treated?
Treatment for coronary artery disease primarily includes lifestyle changes, risk factor management and medications. However, in advanced disease cases, invasive procedures to open the vessel are required. These:
- Angiographically;
- Balloon
- Stent
- Atherectomy (shaving or cutting out the narrowing plaque)
- Lithotripsy balloon (the plaque in the vessel is weakened with ultrasonic waves and opened with a balloon)
- Bladed and cutting balloons (which provide the advantage of opening the lumen by cutting the hard plaques in the vessel)
- Laser (opening severe stenosis in the vein with the help of laser beams)
- It is the addition of a new blood vessel through open heart surgery.
Your physician will talk to you and, if necessary, with colleagues at the heart council about the best treatment option for you and make a plan. It’s important to follow your treatment plan so you can reduce your risk of serious complications from coronary artery disease.
lifestyle changes
Lifestyle changes play a big role in treating coronary artery disease. If we list these changes:
- Do not smoke, e-cigarette or use any tobacco products.
- Eat healthy foods that are low in sodium, saturated fat, trans fat and sugar.
- The Mediterranean diet is a proven way to reduce your risk of heart attack or stroke.
- Exercise: Aim for 30-60 minutes of walking (or other activities, such as cycling) at least five days a week.
- Limit alcohol consumption to 200 grams per week.
By the way, be sure to talk to your doctor before starting a new exercise program. Your doctor will also offer guidance on lifestyle changes tailored to your needs. He or she may suggest smoking cessation options or suggest meeting with a dietitian to discuss healthy eating plans.
Risk factor management
Managing your risk factors for coronary artery disease will help slow or even stop the progression of your disease. You should work with your doctor to manage the following conditions:
- Diabetes.
- Hypertension.
- High cholesterol.
- High triglycerides (hypertriglyceridemia).
- Having a body mass index (BMI) higher than 25. (You can calculate your body mass index by dividing your body weight in kilograms by the square of your height in meters. Kg/height2)
Drug Treatment
Medications help you manage your risk factors, prevent disease progression, and treat symptoms of coronary artery disease. Your doctor may prescribe one or more medications, including:
- cholesterol medications
- Medicines that delay blood clotting (also known as blood thinners)
- Medicines that control blood pressure
- Medicines to reduce chest pain
- These are drugs that prevent the growth of intravascular plaques.
Angiographic Procedures (Balloon/Stent/Atherectomy/Lithotripsy/Laser) and Open Heart Surgeries (Bypass Surgery)
Some people need a procedure or surgery to manage coronary artery disease: Your cardiologist will decide which treatment method to use after making all the necessary examinations and, in advanced risk cases, i.e. if necessary, discussing your situation with the heart council.
1)Percutaneous Coronary Intervention: This minimally invasive procedure has another name: “Coronary Angioplasty”. Your doctor may reopen your blocked artery to ensure adequate blood flow and may also place a stent to help keep your artery open. To this entire procedure; It is called “Percutaneous Coronary Intervention”, “Angioplasty and Stent”, “Percutaneous Revascularization” or most commonly known as “Balloon/Stent Treatment”.
2) Coronary Artery Bypass Grafting (Bypass Surgery): This surgery involves adding a new pathway for your blood to flow around the blockages in the artery. This is usually achieved by removing the vein taken from the leg, the artery in the chest, or the artery in the forearm, and sewing one end to the aortic vein and the other end to the blood flow direction of the stenosis in the coronary artery (since one end of the intrathoracic artery is naturally connected to the main branch of the aorta, it is sufficient to sew the single cut end to the part of the coronary artery after the stenosis). This “detour” restores blood flow to the undernourished part of your heart.
Which method will be suitable and safer for you is determined entirely by your additional diseases, body structure and vascular anatomy. And it should be determined by your heart council, which consists of cardiovascular surgeons and anesthesiologists, as well as cardiologists, when necessary. In the light of current scientific data, some patients gain more advantages from angiographic closed methods, while some patients gain more advantages from open bypass surgery. However, in terms of ratio, in the light of scientific data and experience available almost all over the world, more than 90% of coronary artery patients are successfully treated with angiographically closed methods. The success rate is very high, especially with the technological devices used in recent years (“Atherectomy”, “Lithotripsy balloons”, “Blade balloons”, “Laser” and “High pressure resistant balloons”) and “New generation drug-coated balloons” and “New generation drug-coated stents”.
How long does it take to recover after these treatments?
After angiographic treatments, you can usually return to your normal activities within 1-2 days. However, after bypass surgery, you will stay in the hospital for about a week. And then it will take 6 to 12 weeks for full recovery and return to your normal daily life.
PREVENTION FROM CORONARY ARTERY DISEASE
Can coronary artery disease be prevented?
You can’t always prevent coronary artery disease because some risk factors are beyond your control. But you can reduce your risk of coronary artery disease and help prevent it from getting worse by:
- Stop smoking and using all tobacco products,
- Eat heart-healthy foods (Avoid saturated fat and processed carbohydrates),
- Get enough sleep (at least 7 hours for adults),
- Stay at a weight that is healthy for you (your body mass index should be under 25),
- Learn your heart disease risk,
- Limit alcohol consumption (not to exceed 200 grams per week),
- Exercise (Recommended 150 minutes per week for women, 300 minutes for men),
- Continue taking your medications if started.
PROCESS OF CORONARY ARTERY DISEASE
I have coronary artery disease. What kind of life awaits me?
The person who will make the clearest and best assessment of the course of your disease is your cardiologist. Because the course of the disease varies from person to person. Your doctor will look at the big picture, including your age, medical condition, risk factors, and symptoms. And it will identify and explain all the scenarios that await you ahead. Lifestyle changes and appropriate treatments will increase your chances of a good outcome.
Can coronary artery disease be reversed?
You often cannot completely reverse coronary artery disease. But you can manage your condition and prevent it from getting worse. With current treatment methods, you can live a life as long as you would if you did not have the disease. The tricks for this are to follow your treatment and lifestyle plan in line with your doctor’s recommendations and not to skip your check-ups. Doing this will give you the best possible chance for a long, healthy life.
How should I take care of myself?
The most important thing you can do is to follow your treatment plan. This includes lifestyle changes and medications. Along with treatment, your doctor may also recommend cardiac rehabilitation. A cardiac rehabilitation program is especially helpful for people who have had a heart attack or are living with heart failure. Cardiac rehabilitation can also help you with exercise, dietary changes, and stress management.
Coronary artery disease and mental health
A diagnosis of coronary artery disease may make you think more about your heart and arteries than ever before. This can be tiring and overwhelming. You may worry a lot about your symptoms or what might happen to you. Many people with coronary artery disease experience depression and anxiety. It’s normal to worry when living with a potentially life-threatening condition. However, this worry should not affect your daily life. You can live an active and fulfilling life even when you have heart disease. If your diagnosis is affecting your mental health, you need to talk to a professional counselor. After all, Coronary artery disease is a diagnosis that changes life more or less. You need to take time and make an effort to evaluate all of these and figure out how to feel better both physically and emotionally.
How often should I see my doctor while under surveillance?
Your doctor will tell you how often you need to come for tests or follow-ups, depending on the condition of your disease and the treatment applied, which is most often at intervals of 3, 6 or 12 months. However, you should still contact your doctor even if it is not time for your check-up in some of the following cases:
- If you experience new or changing symptoms such as chest pain, shortness of breath, palpitations, dizziness,
- If your medications have side effects,
- If you have questions or concerns about your condition or treatment plan, you should contact your cardiologist without waiting for your routine checkup.
I have coronary artery disease and in what cases should I go to the emergency room without waiting?
Call 112 if you are experiencing symptoms of a heart attack (Sudden and especially starting at rest, Chest pain; Shortness of breath; Sweating; Back pain; Arm pain; Pain in the upper abdomen or a combination of these symptoms) or Stroke (Loss of sensation in a part of the body; Inability to move some areas; Loss of vision and other senses). These are life-threatening medical conditions that require immediate attention. It may be helpful to print out these symptoms and keep them somewhere you can see them. Also, share your symptoms with family and friends so they can call 911 for you if necessary.
What questions should I ask the doctor I see for coronary artery disease?
1) If you’ve been examined and your doctor hasn’t diagnosed you with coronary artery disease, you should consider asking these questions:
- What are my risk factors for coronary artery disease?
- What can I do to reduce my risk?
- What are the most important lifestyle changes for me?
- Which medications reduce my risk and what are their side effects?
- How long should I use these medications?
2)If you already have Coronary artery disease, here are some useful questions to ask your doctor:
- What can I do to slow the progression of the disease?
- What is the best treatment plan for me?
- What lifestyle changes should I make?
- What medications do I need and what are the side effects?
- Will I need an angiographic or open surgery procedure?
- What will my recovery process be like?
- How should I act and where should I go in case of emergency?
CONCLUSION:
Today, it is possible to live a life without fear of Coronary artery disease as long as you cooperate with your doctor according to modern diagnosis, treatment and follow-up protocols.