Aortic Valve Stenosis
Aortic valve stenosis is a type of heart valve disease, also called heart valve disease. The aortic valve is between the lower left heart chamber and the main artery of the body called the aorta. In aortic valve stenosis, the valve narrows and does not open fully. This reduces or blocks blood flow from the heart to the aorta and the rest of the body.
Treatment of aortic stenosis depends on the severity of the condition. Treatment may include surgery to repair or replace the valve. If left untreated, severe aortic valve stenosis can lead to life-threatening complications.
Symptoms
Aortic valve stenosis ranges from mild to severe. Symptoms usually occur when the valve becomes too narrow. Some people with aortic valve stenosis may not have symptoms for many years.
Symptoms of aortic valve stenosis may include:
- Chest pain or tightness with activity.
- Feeling faint or dizzy, or fainting from activity.
- Shortness of breath, especially during activity.
- Fatigue, especially during times of increased activity.
- Fast, pulsating heartbeat.
Children with aortic valve stenosis may also experience other symptoms, such as:
- Not eating enough.
- Not gaining enough weight.
Aortic valve stenosis can lead to heart failure. Symptoms of heart failure include extreme fatigue, shortness of breath, and swelling in the ankles and feet.
When should you see a doctor?
If you have an irregular heartbeat or other symptoms of aortic valve stenosis, make an appointment with your healthcare provider.
Reasons
To understand the causes of aortic valve stenosis, it can help to know how the heart and heart valves typically work.
The heart has four valves that keep blood flowing correctly:
- aortic valve
- Ax mitral
- tricuspid valve
- lung valve
Each valve has flaps, also called valves, that open and close once during each heartbeat. Sometimes valves do not open and close properly. If a valve does not open and close fully, blood flow is reduced or blocked.
In aortic valve stenosis, the valve between the lower left heart chamber, called the left ventricle, and the main artery of the body, called the aorta, becomes narrow and does not open fully. This narrowing is called stenosis.
When the aortic valve opening narrows, the heart must work harder to pump enough blood to the body. The extra work can cause the lower left heart chamber to thicken. Eventually the heart may weaken.
Causes of aortic valve stenosis include:
- Heart disease present at birth is called congenital heart defect. Some children are born with an aortic valve that has only two protrusions instead of the normal three. If there are only two protrusions, it is called a bicuspid aortic valve. Rarely, one or four protrusions may be present on the aortic valve.
- Calcium buildup in the valve, called aortic valve calcification. Calcium is a mineral found in the blood. As blood moves over the aortic valve, calcium can build up in the valve. Calcium deposits may never cause problems. Aortic valve stenosis, which is associated with advancing age and the accumulation of calcium deposits, usually does not cause symptoms until age 70 or 80. However, in some people, especially those with changes in the aortic valve at birth, calcium deposits can cause the valve to narrow at a younger age.
- Rheumatic fever. This complication of untreated strep throat can damage heart valves. It may cause scar tissue to form on the aortic valve. Scar tissue can narrow the aortic valve opening. It can also create a rough surface where calcium deposits can collect.
Risk factors
Risk factors for aortic valve stenosis include:
- Older age.
- Some heart conditions that are present at birth, called congenital heart defects. An example is the bicuspid aortic valve.
- Long-term kidney disease.
- Heart disease risk factors such as diabetes, high cholesterol and high blood pressure.
- Infections that can affect the heart, such as rheumatic fever and infective endocarditis.
- Radiation therapy to the chest area.
Complications
Possible complications of aortic valve stenosis include:
- Heart failure.
- Paralysis.
- Blood clots.
- August.
- Irregular heartbeats called arrhythmia.
- Infections affecting the heart, such as endocarditis.
Prevention
Some possible ways to prevent aortic valve stenosis include:
- Get a health check when you have a sore throat. Untreated sore throat can lead to rheumatic fever, which can damage heart valves. Strep throat can usually be easily treated with antibiotics. Rheumatic fever is more common in children and young adults.
- Keep the heart healthy. Talk to your healthcare team about your heart disease risk factors. Ask how to prevent and manage them. Risk factors such as high blood pressure, obesity, and high cholesterol may be linked to aortic valve stenosis.
- Take care of your teeth and gums. There may be a link between infected gums, called gingivitis, and a heart infection, known as endocarditis. Endocarditis is a risk factor for aortic valve stenosis.
Diagnosis
To diagnose aortic valve stenosis, a healthcare professional will examine you and ask questions about your symptoms and medical history. The healthcare provider listens to your heart with a stethoscope. If you have aortic valve stenosis, a sound called a heart murmur may be heard.
Tests
Tests can tell if you have aortic valve stenosis. They can also find out the cause and how severe the condition is.
Tests for aortic valve stenosis may include:
- Echocardiogram: Sound waves are used to take pictures of the beating heart. An echocardiogram shows how blood flows through the heart and heart valves. It can tell how severe the aortic valve stenosis is. The test can also show whether the heart muscle is weakened.
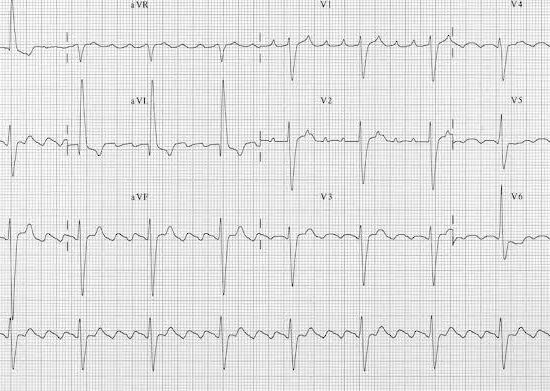
There are different types of echocardiograms. The type you have depends on the information your healthcare team needs. A standard echocardiogram is done from outside the body. An ultrasound device moves over the skin of the chest above the heart. If more details about the heart are needed, a transesophageal echocardiogram may be performed. This type creates pictures of the heart from inside the body. The ultrasound device is connected to a tube that goes down the throat and into the esophagus. - Electrocardiogram (ECG or EKG): This rapid test records the electrical activity of the heart. It shows how the heart beats. Adhesive patches with sensors on them are found on the chest and sometimes on the legs. Cables connect the patches to a computer that displays or prints the results. Your healthcare provider may look for signal patterns related to heart disease or swelling of the heart chambers.
- Chest x-ray: A chest x-ray shows the condition of the heart and lungs. It can show whether the heart is larger than normal, which may occur with aortic valve stenosis. It can also tell if there is calcium buildup in the aortic valve.
- Exercise tests or stress tests: These tests usually involve walking on a treadmill or riding a stationary bike while checking the activity of your heart. Exercise tests show how your heart responds to physical activity and whether valve disease symptoms occur during exercise. If you cannot exercise, you can take medications that affect the heart, such as exercise.
- Cardiac computed tomography (CT) scan: This test uses several X-rays to create detailed images of the heart and heart valves. The test may be done to check the size of the aorta and take a closer look at the aortic valve. A CT scan may be done to see how much calcium has built up on the valve. It can also show how severe the aortic valve stenosis is.
- Cardiac magnetic resonance imaging (MRI) scan: Cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart. This test can show the size of the aorta. It can be used to find out how serious aortic valve stenosis is.
- Heart catheterization: This test is not often used to diagnose aortic valve disease. However, it may be done to see how severe aortic valve disease is or to diagnose the condition if other tests fail. In this test, the doctor inserts a thin, flexible tube into a blood vessel, usually in the groin area or arm, and directs it to the heart. Cardiac catheterization may also be used before aortic valve surgery to ensure that the heart arteries are not blocked.
After the test confirms the diagnosis of aortic valve disease, your healthcare provider can tell you the stage of the disease. Staging helps your healthcare team choose the most appropriate treatment.
Heart valve disease is divided into four basic groups:
- Stage A: At risk. There are risk factors for heart valve disease.
- Stage B: Gradual. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms, but valve disease is serious.
- Stage D: Symptomatic severe. Heart valve disease is serious and causes symptoms.
The stage of heart valve disease depends on many things, including symptoms, severity of disease, structure of the valve or valves, and blood flow in the heart and lungs.
Treatment
Treatment of aortic valve stenosis depends on the symptoms and severity of the condition. Aortic valve stenosis ranges from mild to severe.
If you have no symptoms or only mild symptoms, you may only need regular checkups. Some people need medications to treat valve disease symptoms or reduce the risk of complications.
Other treatments for aortic valve disease may include:
- Heart-healthy lifestyle changes. Eat healthy, exercise regularly, stay active and don’t smoke.
- Medicines used to treat symptoms or reduce the risk of complications.
- Surgery to correct or replace the valve.
Medicines
Some people with aortic valve stenosis may need medications to treat symptoms or reduce the risk of complications. For example, medications can be used to:
- Lower blood pressure.
- Prevent irregular heartbeats.
- Remove excess fluid from the body to reduce the burden on the heart.
Surgery or other procedures
Even if you don’t have symptoms, you may eventually need surgery to repair or replace the narrowed aortic valve. Aortic valve surgery can be done at the same time as other types of heart surgery.
Surgery to repair or replace the aortic valve is usually done through an incision in the chest. Less invasive approaches may be available. Ask your healthcare provider which type of aortic valve treatment is best for you.
Surgery and procedures for aortic valve stenosis include:
- Balon valvüloplasti: This treatment helps open a narrowed valve. It can be performed in infants and children with aortic valve stenosis. In adults, the aortic valve tends to narrow again after treatment. For this reason, it is usually only done if an adult is too sick to have surgery or if an adult is waiting for a valve replacement.
In balloon valvuloplasty, the doctor inserts a thin tube into a blood vessel in the arm or groin and directs it to the aortic valve. Once in place, a balloon at the end of the tube is inflated. This allows the valve opening to be wider. The balloon is deflated. The tube and balloon are removed. - Aortic valve replacement: Aortic valve replacement is often needed to treat aortic valve stenosis. In an aortic valve replacement, the surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue. The tissue valve is called biological tissue valve.
Sometimes the aortic valve is replaced with a person’s own lung valve, called a pulmonary valve. The pulmonary valve is replaced with a valve of biological lung tissue taken from a deceased donor. This more complex surgery is called the Ross procedure.
Biological tissue valves deteriorate over time and may eventually need to be replaced. People with mechanical valves must take blood-thinning medications for life to prevent blood clots. Talk to your healthcare team about the benefits and risks of each type of valve. - Transcatheter aortic valve replacement (TAVR): TAVR is an option to open heart valve surgery. Small incisions and a thin, flexible tube called a catheter are used to replace the aortic valve. During TAVR, the surgeon replaces the narrowed aortic valve with a valve made from cow or pig tissue. If you are at moderate or high risk of complications from surgical aortic valve replacement, TAVR may be an option. Ask your healthcare team about your options.
During TAVR, the surgeon inserts a tube into the blood vessel and directs it to the heart. A replacement valve made of cow or pig tissue goes through the tube to the aortic valve area. A balloon at the end of the tube inflates, pushing the new valve into place. Some valves can self-expand. The tube is removed. Surgeons may also use tubes called catheters to insert a replacement valve into a biological tissue valve that is no longer working properly. - Aortic valve repair: Surgeons can fix the aortic valve by separating the valve flaps that stick together. However, valve repair is rarely used in the treatment of aortic valve stenosis. Generally, aortic valve stenosis requires aortic valve replacement.
Lifestyle and home remedies
Try these tips to help prevent or slow aortic valve stenosis and other types of heart disease.
- Do not smoke or use tobacco: Smoking is a major risk factor for heart disease. If you smoke and cannot quit, talk to your care team about programs or treatments that may help.
- Eat a heart-healthy diet: Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish and whole grains. Limit salt and saturated fats.
- Maintain a healthy weight: Lose weight if you are overweight or obese. Losing just a few pounds can help reduce heart disease risk factors. Ask your healthcare provider what weight is best for you.
- Exercise regularly: Exercise helps manage weight and control risk factors for heart disease. Exercise at least 30 minutes a day on most days of the week. Talk to your healthcare team about the amount and type of exercise that is best for you.
- Manage stress: Learn ways to help reduce emotional stress. Some ideas are to exercise more, practice mindfulness, or connect with others in support groups.
- Check blood pressure, blood sugar and cholesterol: Make lifestyle changes and take medications as directed. Get regular health checks.
- Limit alcohol: If you choose to drink alcohol, do so in moderation. For healthy adults, this means one drink per day for women and two drinks per day for men.
- Night night: Poor sleep can increase the risk of heart disease and other health problems. Adults should aim for 7 to 9 hours a day.
If you have aortic valve stenosis, your healthcare team may recommend that you limit strenuous activities to prevent your heart from overworking.
Pregnancy and aortic valve disease
If you have aortic stenosis and are considering becoming pregnant, it is important to talk to your healthcare team about your plans. Together, you can talk about the safety of medications and whether you need treatment for aortic valve stenosis before getting pregnant.
People with heart valve disease, such as aortic valve stenosis, usually need close monitoring by a healthcare professional during pregnancy. If you have severe aortic stenosis, healthcare professionals may tell you not to get pregnant due to the risk of complications.