Evidence-Based Tests for Coronary Artery Disease
Evidence-Based Tests for Coronary Artery Disease (CAD) in Asymptomatic Adults
Why is Cardiovascular Health and Screening Important?
Most heart attacks occur over time when fat, cholesterol and lime (calcium) deposits called “plaque” form on the inner wall of the arteries that feed the heart (coronary arteries). This condition is called Coronary Artery Disease (CAD). High cholesterol, high blood pressure, diabetes, smoking, unhealthy diet, excess weight and inactivity are the most important risk factors that accelerate plaque accumulation. Therefore, the first step in protecting cardiovascular health and detecting possible diseases early is to know and control these risk factors. Even people who do not show any symptoms (chest pain, shortness of breath, etc.) may sometimes need further testing, but it is very important to follow an evidence-based approach to when and to whom these tests should be performed [1, 2]. This guide will help you understand which tests may be suitable for whom.
1. What Should Be Considered Before Tests?
- Primary Prevention First: All current health guidelines agree that controlling known risk factors (cholesterol, blood pressure, smoking, weight, poor diet, lack of exercise) prevents more heart attacks than any screening test can detect [2]. Therefore, routine CAD “screening” is not recommended in the low-risk general population.
- Risk Assessment Before Imaging: Imaging tests (CT, angiography, etc.) are not performed on everyone. These tests are considered for selected adults whose 10-year cardiovascular disease risk is found to be undetermined or intermediate as a result of standard risk calculation methods (such as SCORE2 used in Türkiye and Europe or Pooled Cohort Equations used in the USA) [2, 3]. The term Atherosclerotic Cardiovascular Disease (ASCVD) Risk refers to your probability of experiencing arteriosclerosis-related events such as heart attack and stroke, and is usually calculated as a percentage.
- Shared Decision Making: None of the tests mentioned below carry a “must do” (Class I) recommendation for asymptomatic individuals. At best, they are at the “might be reasonable to do” level (Class IIa-IIb). Therefore, before having any test, it is very important to discuss with your doctor the potential benefits of the test, its risks (e.g. radiation dose), possible side effects, cost, and whether the test result will actually change your treatment [4].
2. Routine Health Assessments for Every Adult
These checks provide the basis for determining whether any further testing is needed:
| Control | Starting Age | Frequency | Why is it important? | Reference |
| Lipid Profile (Blood Fats) + ASKVH Risk Calculation | ≥20 years of age (risk calculation every 5 years under the age of 40, every 4-6 years for those aged 40-75) | Read the note below | The basis for all other decisions; determines statin (cholesterol medication), blood pressure and lifestyle treatments. | [2] |
| Blood Pressure Measurement | ≥18 years of age at every doctor visit | At every examination | High blood pressure alone is an important cause of CAD. | [2] |
| Diabetes Screening (Fasting Blood Glucose / HbA1c) | ≥35 years (USPSTF recommendation) [5] | Every 3 years | The presence of diabetes automatically puts the patient in the ‘high risk’ category. | [5] |
| Family History, Smoking, Body Mass Index (BMI) | At any age | At every examination | According to ACC/AHA guidelines, these are factors that increase risk. | [2] |
Figure 1: Important Note: At this stage, no routine imaging (film, CT, etc.) or stress testing is recommended for people who are asymptomatic.
3. Non-Imaging Functional Tests
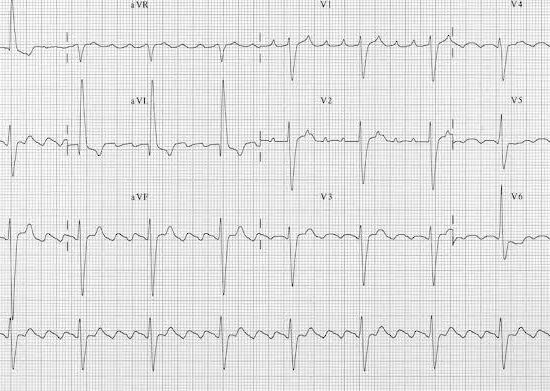
Figure 2: Example of an ECG
| Test | Guide Opinion | For Whom Can It Be Considered (If Necessary)? | Key Information | Reference |
| ECG (Electrocardiogram) | It is not routinely recommended in low-risk individuals; There is insufficient evidence at high risk [6]. | Only if the 10-year risk of ASCVD is very high and the outcome would change pre-operative or sports-leaving decisions. | There is no evidence that it reduces heart attacks; False positive results may lead to unnecessary action. | [6] |
| Stress ECG (Treadmill Test) ± Stress Imaging | It is not recommended in the general asymptomatic population [4, 7]. | Selected individuals aged ≥40 years, with multiple risk factors, and working in physically demanding professions (pilot, firefighter, etc.). | The rate of a positive test correctly predicting the disease is ≤50%; There are no studies showing that it reduces heart attacks. | [4, 7] |
Summary: Functional tests (ECG, Stress ECG) are generally used only for special situations such as occupational or preoperative evaluation, they are not suitable for screening the average person.
4. Imaging-Based Anatomical Tests (Tests Showing Vascular Structure)
4.1 Coronary Artery Calcium (CAC) Scoring (Non-contrast CT, ~0.7 mSv Radiation)

Figure 3: CT is used for coronary calcium scoring. Calcium appears white in the coronary arteries.
What is CAC Score?
This is a low-dose computed tomography (CT) scan and measures the amount of calcium (lime) deposited in the vessels feeding the heart. Calcium is an indicator of atherosclerosis plaque. The radiation dose is quite low (less than approximately one year of natural background radiation) [8].
When to Use?
In adults aged 40–75 years, if the estimated 10-year risk of ASCVD is moderate (7.5%–20%) and the decision to start a statin (cholesterol-lowering drug) is uncertain (ACC/AHA 2019, Class IIa recommendation) [2].
If the calculated risk is borderline (5%–7.4%) and there are additional risk-increasing factors (family history of heart disease at an early age, metabolic syndrome, chronic inflammatory disease, etc.) [2].
When Not to Use?
If the 10-year risk is <5% (low) (statins are not usually given).
If the 10-year risk is >20% (high) (high-dose statin is already recommended). In these cases, the test result does not change the treatment decision.
Evidence:
– MESA study: CAC score changed the risk class of 25-40% of intermediate-risk adults. The 10-year risk of heart attack was found to be <1% in those with a CAC score of 0 [9].
-2021 systematic review (JAMA Intern Med): In an analysis of 17 studies, the CAC score was shown to provide an 18-25% improvement in more accurately classifying risk in addition to traditional risk factors [8].
CAC Score Results and Interpretation:
| Score Value | Meaning | Recommended Approach |
| 0 | No detectable calcium. | Statin therapy may be postponed (except for smokers, diabetics, those with a strong family history). Repeat CAC may be considered after 5-10 years. |
| 1–99 | Mild plaque burden. | Moderate-intensity statin therapy is recommended, especially if age ≥55 years. |
| ≥100 or ≥75% percentile for age | Moderate-High plaque burden. | Considered high risk: High-intensity statins should be started, blood pressure-cholesterol-lifestyle targets should be tightened. If the risk of bleeding is low, aspirin may be considered. |
| ≥400 | Too high plaque burden. | He should be referred to a cardiologist. The severity of the stenosis in the vessels or its effect on blood flow (ischemia) can be evaluated with a functional test (stress echocardiography/SPECT) or Coronary CT Angiography (CCTA). If necessary, invasive angiography may be considered. |
Radiation Risk: The radiation dose in this test is low (<1 mSv). The risk of developing cancer due to this is theoretically less than 1 in 10,000.
4.2 Coronary CT Angiography (CCTA) (2–4 mSv Radiation with Modern Devices)

Figure 4: Coronary Ct Angiography (CCTA)
What is CCTA? This test is a computerized tomography method performed by administering contrast material (dyed drug) intravenously and showing the internal structure of the coronary arteries in detail. It involves a higher radiation dose than CAC scoring.
Guideline recommendations: No place in general population screening (Class III – No Benefit/May Be Harmful). It is often used to evaluate patients with symptoms such as chest pain [4].
Evidence:
FACTOR-64 Study: CCTA scanning in 900 patients with diabetes did not reduce heart attacks or death within 4 years [10].
DANCAVAS Study: The effect of screening with CCTA and other tests on men aged 65-74 was found to be neutral on overall mortality rates. Although a small risk reduction was seen in the 65–69 age group, this was offset by an increased risk of intracranial bleeding [11].
Conclusion: CCTA should not be used for screening purposes in asymptomatic individuals outside of research protocols. Sometimes when a risk assessment such as CAC is required, it may be preferred if the patient is young. Because, in young patients, atherosclerotic plaques are more lipid (fat)-based and calcium accumulation may not have occurred yet.
4.3 Carotid Intima-Media Thickness (CIMT) / Carotid Ultrasound

What is CIMT? It is an ultrasound test that measures the wall thickness of the jugular vein (carotid artery) in the neck.
Guideline recommendation: Guidelines oppose the routine use of ultrasound to screen for carotid stenosis in asymptomatic adults [12]. CIMT measurement adds little discriminatory power over and above traditional risk factors [13] .
Conclusion: Not recommended for CAD screening.
4.4 Ankle-Brachial Index (ABI)

What is ABI? It is a simple test that evaluates possible blockage in the leg veins by measuring the blood pressure in the legs and arms.
Guideline recommendation: When used as a stand-alone CAD screening, its net benefit is inconsistent across studies and the evidence is inconclusive [14].
Conclusion: Not recommended for routine CAD screening.
5. Biomarkers and Genetic Tests (Does Not Diagnose, May Help)
These tests alone do not diagnose CAD, but they can help decide, especially in people at moderate risk:
| Adverb | Level of Evidence | When Can It Be Measured? | How Can It Change Treatment? | References |
| High Sensitivity CRP (hs-CRP) | It indicates low-level inflammation in the body. It is associated with the risk of heart attack, but has a weaker connection with CAC [15, 16]. | If the risk of ASCVD is between 5% and 20% and there is suspicion of inflammation. | If ≥2 mg/L, focus on treating underlying metabolic/inflammatory conditions; may support the decision to start a statin. | [15], [16] |
| Lipoprotein(a) [Lp(a)] | A specific type of cholesterol that is genetically determined and is a causal risk factor for CAD. ACC/AHA recommends measurement once in a lifetime [17]. | In cases such as a family history of CAD at an early age or being of South Asian origin. | LDL-Cholesterol target can be lowered; Lp(a)-lowering treatments may be considered in the future. | [17] |
| Polygenic Risk Scores (PRS) | Calculates the effect of more than one gene on CAD risk. It is in the research phase and is not yet recommended in the guidelines. | In selected families with CAD at a very early age. | Its clinical benefit is still under evaluation. |
6. Recommended Integrated Screening Approach
- Calculate Risk: Calculate your 10-year ASCVD risk calculate (SCORE2 etc.) and additional factors that increase the risk (family history, cigarette etc.) determine.
- Low Risk (<5%): Lifestyle recommendations are given, no viewing required.
- Medium Risk (7.5%–20%) or Borderline Risk (5-7.4%) + Risk Enhancers: Talk to your doctor about the CAC score option. Especially in the middle Statin is already recommended for risk, but if you are not sure about using it, the statin decision may become clear depending on the test results.
- High Risk (≥20% or 40-75 years old with diabetes or LDL Cholesterol ≥190 mg/dL): High-intensity statin therapy and aggressive risk factor control are initiated. Unless symptoms develop no initial imaging is usually required.
- Abnormal Test Result: If CAC score is ≥400 or CAC If the score is inconsistent with the clinical condition/other tests: A functional test (such as stress echocardiography/SPECT) or CCTA can be performed. If tests show your heart If serious blood flow disorder (ischemia) affecting more than 10% or stenosis of more than 70% is detected, referral to a cardiologist and If necessary, invasive angiography is considered. There is a very important thing to remember here that even if there is stenosis, the main coronary artery (LMCA) If there is no stenosis or heart failure, the only benefit of stent or bypass is It is symptomatic. Therefore, drug treatment is recommended instead of stent or bypass in people without symptoms, even if they have severe stenosis.
- Retest: If the initial CAC score is 0 and after 5-10 years if risk status or treatment thresholds may change over time Repeat CAC may be considered. Otherwise, if there are no symptoms, repeat routine viewing is not recommended.
7. Special Situations
- Diabetes Patients (≥40 years): If the disease duration is >10 years and If there are no other high-risk features, the CAC score may be considered. The benefit of routine CCTA screening has not been demonstrated (FACTOR-64 study) [10].
- Middle-Aged Men Working Heavy Work (Pilots, Firefighters, etc.): CAC score or stress test may be requested due to institutional requirements, but medical benefit has not been proven – decision should be made on an individual basis.
- Adults Over 75: Data is limited in this age group. Since age itself generally brings a high risk, it may be more logical to start drug protection (statin, etc.) directly without imaging in most people.
8. Research and Developing Methods (Not in the Guides Yet)
- Calculation of CAC score with artificial intelligence from low-dose CT scans taken for lung screening (opportunistic screening).
- Multi-omics / Proteomic Risk Scores: Predicts risk by looking at genes, proteins and other molecules, shows promise in the early stages, but there is no evidence yet that it improves outcomes (there are many ongoing studies).
9. Summary for Physicians
- Do the simple things first: Blood fats, blood pressure, blood sugar control and healthy lifestyle advice.
- Reserve CAC scoring for “gray area” patients for whom the risk-benefit balance of long-term statin therapy is uncertain (intermediate risk group).
- Avoid using CCTA, resting ECG, or stress tests as general screening tools: They have not been shown to reduce heart attack rates and expose patients to radiation, cost, and the risk of false-positive results.
- Act decisively when test results are abnormal: maximally lower LDL-Cholesterol and blood pressure, aim to treat obesity/diabetes, consider low-dose aspirin (if bleeding risk is low) but do not routinely use preventive therapy, and refer for further testing (ischemia testing, invasive angiography) only when non-invasive testing shows high anatomical or ischemic burden.
10. Summary for Patients and Families:
- Most heart attacks are caused by fatty “plaque” that slowly builds up in the arteries of the heart. The best way to prevent this is to control cholesterol, blood pressure, blood sugar, weight and quit smoking – not by taking lots of films and tests. Detecting plaque through early screening tests and installing a stent does not reduce the risk of a heart attack in the future, so it is not recommended.
- A quick CT scan, called a Calcium Score (CAC), can help people who are neither low nor high risk — those “caught in the middle” — decide whether they should start medications such as statins.
- More advanced imaging tests (such as CT Angiography) or stress tests are almost never helpful for people who feel well and have no symptoms, and can sometimes lead to unnecessary procedures.
- First discuss your personal risk figures with your doctor; Only use tests if the result will change your next step.
Abbreviations:
ABI: Ankle-Brachial Index
ACC: American College of Cardiology
AHA: American Heart Association
ASCVD: Atherosclerotic Cardiovascular Disease
CT: Computed Tomography
CAC: Koroner Arter Kalsiyum (Coronary Artery Calcium)
CCTA: Coronary CT Angiography
CIMT: Carotid Intima-Media Thickness
EKG: Electrocardiogram
ESC: European Society of Cardiology
hs-CRP: High Sensitivity C-reactive Protein
CAD: Coronary Artery Disease
Lp(a): Lipoprotein(a)
RCT: Randomized Controlled Trial
USPSTF: U.S. Preventive Services Task Force
References:
-
European Society of Cardiology (ESC). (2021). ESC Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal, 42(34), 3227–3337. (Genel korunma ve risk değerlendirmesi ilkeleri)
-
Arnett, D. K., Blumenthal, R. S., Albert, M. A., Buroker, A. B., Goldberger, Z. D., Hahn, E. J., … & Ziaeian, B. (2019). 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 140(11), e596-e646.
-
SCORE2 working group and ESC Cardiovascular risk collaboration. (2021). SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. European heart journal, 42(25), 2439-2454.
-
Doherty, J. U., Kort, S., Mehran, R., Schoenhagen, P., Soman, P., & Dehmer, G. J. (2024). ACC/AHA/ASE/ASNC/ASPC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2024 Multimodality Appropriate Use Criteria for the Detection and Risk Assessment of Chronic Coronary Disease. Journal of the American College of Cardiology, 83(11), 1085-1112. (Testlerin uygun kullanımı ve ortak karar verme)
-
US Preventive Services Task Force. (2021). Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA, 326(8), 736-743.
-
US Preventive Services Task Force. (2018). Screening for Cardiovascular Disease Risk With Electrocardiography: US Preventive Services Task Force Recommendation Statement. JAMA, 319(22), 2308–2314.
-
Gibbons, R. J., Balady, G. J., Bricker, J. T., Chaitman, B. R., Fletcher, G. F., Froelicher, V. F., … & Smith Jr, S. C. (2002). ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation, 106(14), 1883-1892. (Efor testi önerileri – 2024 AUC ile teyit edildi)
-
Bell, K. J. L., White, S. R., Hassan, O., Jones, R., D’Este, C., Glasziou, P., … & Irwig, L. (2022). Evaluation of the Incremental Value of a Coronary Artery Calcium Score Beyond Traditional Cardiovascular Risk Assessment: A Systematic Review and Meta-analysis. JAMA Internal Medicine, 182(6), 634–642.
-
McClelland, R. L., Chung, H., Detrano, R., Post, W., & Kronmal, R. A. (2006). Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation, 113(1), 30-37. (MESA Çalışması CAC verileri)
-
Muhlestein, J. B., Lappé, D. L., Lima, J. A., Rosen, B. D., May, H. T., Knight, S., … & Anderson, J. L. (2014). Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA, 312(21), 2234-2243.
-
Lindholt, J. S., Søgaard, R., Rasmussen, L. M., Mejldal, A., Lambrechtsen, J., Steffensen, F. H., … & Diederichsen, A. C. P. (2022). Five-Year Outcomes of the Danish Cardiovascular Screening (DANCAVAS) Trial. New England Journal of Medicine, 387(15), 1385-1394.
-
US Preventive Services Task Force. (2021). Screening for Asymptomatic Carotid Artery Stenosis: US Preventive Services Task Force Recommendation Statement. JAMA, 325(5), 476-481.
-
Den Ruijter, H. M., Peters, S. A., Anderson, T. J., Britton, A. R., Dekker, J. M., Eijkemans, M. J., … & Grobbee, D. E. (2012). Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA, 308(8), 796-803.
-
US Preventive Services Task Force. (2018). Screening for Peripheral Artery Disease and Cardiovascular Disease Risk Assessment With the Ankle-Brachial Index: US Preventive Services Task Force Recommendation Statement. JAMA, 320(2), 177–183.
-
Emerging Risk Factors Collaboration. (2010). C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. The Lancet, 375(9709), 132-140.
-
Lakoski, S. G., Greenland, P., Wong, N. D., Schreiner, P. J., Herrington, D. M., Kronmal, R. A., … & Criqui, M. H. (2007). Coronary artery calcium scores and risk for cardiovascular events in women classified as “low risk” based on Framingham risk score: the Multi-Ethnic Study of Atherosclerosis (MESA). Archives of internal medicine, 167(22), 2437-2442. (hs-CRP ve CAC ilişkisi)
-
Grundy, S. M., Stone, N. J., Bailey, A. L., Beam, C., Birtcher, K. K., Blumenthal, R. S., … & Yeboah, J. (2019). 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 139(25), e1082-e1143. (Lp(a) ölçümü önerisi)